Board Review
All residency graduates are expected to appear for and successfully complete the ABIM Internal Medicine Certifying Exam in their first attempt, immediately following training.
- A highly interactive Board Review session is conducted throughout the academic year, attended by residents during their clinic week. The program leadership facilitate interactive sessions using materials from the American College of Physicians Medical Knowledge Self Assessment Program (MKSAP) and other resources.
- An annual In-Training Examination is scheduled for all residents enrolled in the program and results are used to drive curricular changes and self-directed study plans.
Evidence Based Medicine (EBM) Course
We recognize the importance of a solid theoretical understanding of the principles of evidence based medicine and its practical applications in the clinical setting. Accordingly, an interactive weekly journal club and a longitudinal EBM course for all residents remains an integral part of our program.
Residents present current and landmark journal articles during our weekly journal club moderated by faculty with expertise. Discussions involve study design, research methodologies, statistical principles and clinical applicability of study outcomes.
The small group discussion-style EBM sessions incorporated into our clinic week curriculum provide a foundation in formulating clinical questions, developing effective research strategies, and critically appraising the literature.


Quality Improvement and Patient Safety (QIPS) Curriculum
Continuous improvement processes are integral to healthcare quality and outcomes. Our integrated ambulatory health systems science curriculum incorporates longitudinal quality improvement initiatives, patient safety education and research.
Our QI curriculum has been well established over the past 5 years. All residents participate in both a didactic and experiential components of the QI curriculum during their ambulatory clinic blocks. They work in multidisciplinary teams on QI projects directed at improving the care of a defined patient population in their practice.
The residents meet with their facilitator weekly to discuss the basic concepts of root cause analysis, PDSA cycle, pay-off priority matrix, and measurement of standarized quality outcomes. Scholarly output, in the form of posters and publications, related to QIPS is encouraged. Data from the academic hospitalist group and the clinic setting is shared with residents.
The Patient Safety component of the curriculum engages residents in didactic sessions on basic patient safety and high reliability organization principles, high value care, and an understanding of heuristics. The residents are encouraged to use the knowledge gained to review and present cases at morbidity & mortality conferences and at patient safety reviews using the root cause analysis (RCA) format.
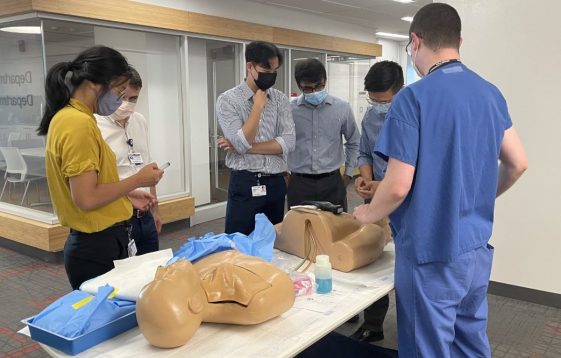
Pocus Curriculum

Resident as Teacher
Acknowledging the Latin etymology of “doctor”, the program expects residents to develop effective teaching skills. Didactic sessions aimed at reviewing teaching techniques and methods for effective delivery of feedback to all learner groups are incorporated into the annual ambulatory curriculum. On the floors, resident led teaching rounds precede daily attending rounds, provide opportunities to demonstrate and review physical exam findings and explore clinical reasoning strategies. During clinic week, residents lead various aspects of the ambulatory curriculum, mentor junior housestaff to optimize EBM skills, and lend guidance on research projects. The Arnold P. Gold foundation and the program honor the efforts of our best resident teachers on an annual basis.
Medical students are a constant presence on the wards and in the subspecialty clinics at RWJUH and Princeton. Second year students learn physical diagnosis skills, third year students complete clinical clerkships, and fourth year students serve as sub-interns. In addition to learning the science of medicine, professional values, attitudes and behaviors are influenced and nurtured by our resident role models.
Community Service Program and Global Health Opportunities
An outgrowth of our Humanism and Professionalism Council established in 1998, this resident-run initiative works in conjunction with the community outreach departments at both our teaching hospitals and through various local organizations.
Residents volunteer time for a variety of activities including:
- Presentations to a wide array of community groups on prevention, detection and treatment of various diseases
- Fund Raising Activities: Diabetes Walk, Cancer Walk-a-thon’s, Thanksgiving Turkey Drive, Back to School Suppiles
- Preventive Medicine: Education and Screening Fairs in collaboration with Rutgers Universtiy students
- Global Health opportunities with Princeton faculty
- Practice Tailoring Global Health Elective
Humanism and Professionalism Council
Created in 1997, the Humanism and Professionalism Council was the Department of Medicine’s response to the ABIM Project Professionalism. The purpose of the council is to oversee educational programs that enhance the knowledge, skills, attitudes, and behaviors of residents and fellows which are essential to continuing medical professionalism. The council meets quarterly and makes recommendations regarding policies, procedures, and standards relevant to medical professionalism. Members include the residency program director and associate directors, faculty, chief residents, elected fellows and residents, medical students, nurses, and chaplains.
This Council conducts a periodic needs assessment to formulate the part of our curriculum known as, “The Art of Medicine”. The curriculum for these sessions includes: professional etiquette, informed consent, patient counseling, palliative care discussions, cross cultural medicine, social media use and misuse, conflict resolution, empathy, altruism and wellness, implicit bias and structural racism. These sessions are conducted in a variety of formats such as lectures, panel discussions, role playing and clinical vignettes or zoom sessions.
Practice Tailoring Rotations
Time may be granted to residents who choose to develop a customized plan to meet personal career goals. For example, residents may focus on such areas as clinical informatics, drug development, business of medicine, or medical education. Such programs require advanced planning by exceptionally motivated residents.